podcast
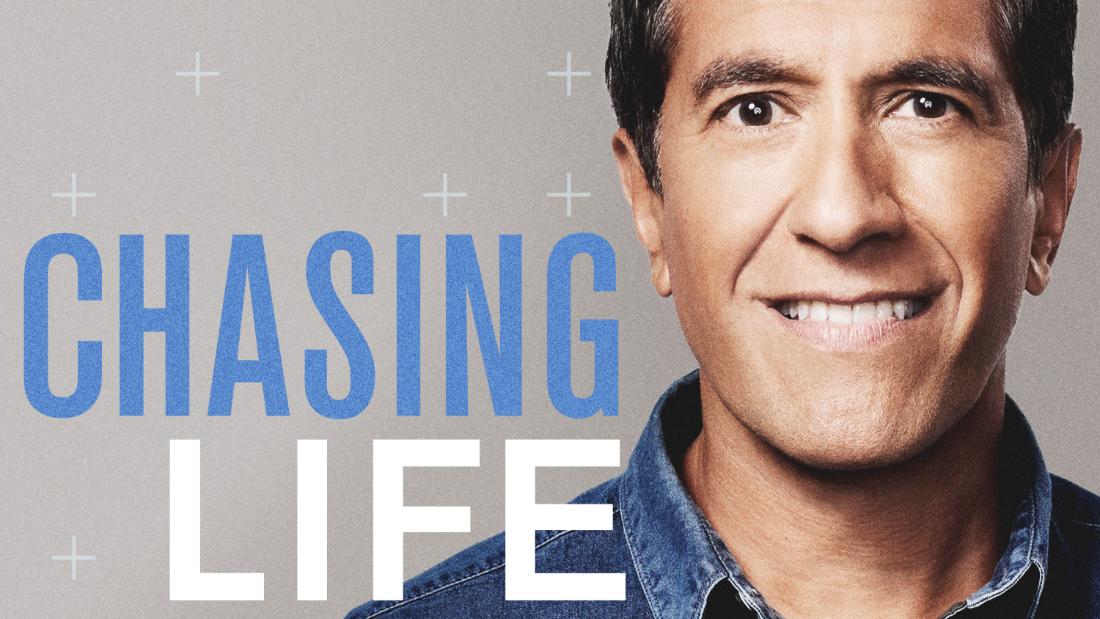
Did you know that some people can taste colors and others have a hard time recognizing faces? This season on Chasing Life, Dr. Sanjay Gupta takes listeners beyond the basics of sight, sound, smell, taste and touch to explore unique sensory experiences. Discover why psychedelics might change your worldview, how animals perceive differently than humans, and how biases in taste might impact the future of food production.
Join us each week to marvel at how the rich landscape of sensory perception shapes our understanding of the world.

Pain is a Four-Letter Word Oct 18, 2022
How do you treat a disease where the cause is unknown and each patient’s symptoms are unique? CNN’s Chief Medical Correspondent Dr. Sanjay Gupta talks to pain expert Dr. Carmen Green about what causes chronic pain, how it can be treated, and which patients are more likely to get care. Plus, meet a man who feels no pain and a woman who figured out how to cope with hers. This episode originally aired in November 2021.
Dr. Sanjay Gupta
00:00:00
Hey there. It’s Sanjay. You know, I’ve been thinking a lot about pain recently, like love and joy. Pain is an integral part of the human experience. At the beginning of the season, I talked with science writer and author Ed Yong about pain being considered one of our senses. And like any other sense, it’s subjective. It is more of an experience than a sensation. The pain that you feel. That’s what happens when your brain processes the information from a type of neuron called the Nociceptors. A nociceptor detects potentially damaging sensations. Think a hand touching a hot stove or a foot stepping on a tack, but it’s a lot more than that. As a neurosurgeon, I deal with pain a lot in my line of work. We often ask patients to rate their pain on a scale of 1 to 10. It’s hard to do, and it can even change in that same patient from moment to moment. Oftentimes, we try to speculate how much pain someone might have based on an MRI scan of an injured joint or an organ. But it is hard to quantify and sometimes hard to fix completely and permanently. All of us – patients, doctors, society, we all have a hard time dealing with understanding how to quantify the experience of pain. So today I decided to reshare an episode we did last year about pain. What happens if you can’t feel it. And if pain feels different for every one of us, how do we treat it? Thanks for listening.
I was an infant when my parents had a feeling that something was wrong. I was teething. And what happened was I had chewed off the the front portion of my tongue.
Dr. Sanjay Gupta
00:01:50
Imagine not being able to feel pain. This is what life is like for Steve Pete.
The majority of my early childhood was spent either in a hospital room or wearing a cast. I think I want to say I’ve probably had around ninety to a hundred broken bones so far in my life. It was constant injury upon injury from things as small as cut myself with a knife, up to having bones just kind of tear through my flesh.
Dr. Sanjay Gupta
00:02:18
Steve has this rare neurological condition. It’s called congenital insensitivity to pain. At 40 years old, he’s cut himself many times while cooking. But the thing is, he never notices it until he sees the blood. He once broke his foot, but didn’t realize it until his wife asked about the bruising. So I was curious, when he does get injured, what is he actually feeling then, if not pain?
I’ll feel the nerves in my body like signaling. Almost like electrical wiring in a way, how it’s sending that electrical pulse. So I feel like this electrical current pulsating from my left knee down to my foot, then back out.
Dr. Sanjay Gupta
00:03:06
That experience that Steve just described actually gives us some really interesting insight into the mechanics of pain.
When you’re experiencing a painful situation, pain is like the loudest voice in the room it’s just screaming in your ears. You’re not feeling what’s going on with your body that is signaling that response. So I’m feeling as I’m able to feel everything that’s going on under that loud, painful, noisy surface.
Dr. Sanjay Gupta
00:03:36
It’s fascinating to think about. You see pain alerts most of us to harm or that something is wrong, that’s so that we can avoid dangerous or damaging situations. But Steve had to learn the hard way.
So by this point, I’m pretty familiar with like how much force is needed to break a bone or how much pressure from a knife is too much. This can cause me to cut my flesh or how much heat is going to cause what type of burn to my body.
Dr. Sanjay Gupta
00:04:10
Now, most of us aren’t like Steve. Pain is a part of our lives. But as a culture, I have to say, we’re not very good at talking about it. We’re often told no pain, no gain, and we often struggle to find the words to meaningfully communicate our own pain or to help others in theirs. On today’s episode, we’re going to explore how pain works, how we can best treat it, and why it’s too often swept under the rug. I’m Dr. Sanjay Gupta, CNN’s chief medical correspondent. And this is Chasing Life.
Dr. Sanjay Gupta
00:04:52
From mild discomfort to off the charts agony. We wanted to hear about some of your more unexpected experiences with pain.
One time I was at work and I held a legal file in my hand and I bent down to pick something up and the legal file gave me a paper cut on my eyeball.
I’m going 3000 miles per hour chasing my brother, and I smack dead into the glass door. Thank God it did not shatter and I did not go through it. But I knocked myself out cold.
I was trying to customize the lacrosse head of mine with my my old Boy Scout Swiss Army knife slipped and split my finger in half.
I was standing on a chair and I fell very hard on my side and I broke myself.
So when I was younger, I ran into one of those cement poles, totally bust my head, blood everywhere. Went home, the next day, I got five stitches. I’m okay.
Dr. Sanjay Gupta
00:05:59
For starters, most pain can be categorized as either acute or chronic.
Dr. Carmen Green
00:06:04
Well, there’s actually a lot of people who will talk about pain, like how much it hurts. But the people who’ve defined this as unpleasant, sensory and emotional experience.
Dr. Sanjay Gupta
00:06:16
That’s Dr. Carmen Green. She’s one of the top pain experts in the country and the dean of the City University of New York School of Medicine.
Dr. Carmen Green
00:06:25
The pain that continues to persist beyond three months, beyond what we call an acute period, is what we talk about as chronic pain. And that’s the one that’s the most disabling and the most problematic for people because it impacts all aspects of their health and well-being.
Dr. Sanjay Gupta
00:06:41
Chronic pain affects between 50 and 100 million Americans. Look, I think we can intuitively understand the evolutionary benefits of acute pain. If there’s a hot stove and you touch it, you burn your hand, you’re going to learn not to do that again. But I’ve often wondered what is the real point from an evolutionary standpoint to chronic pain?
Dr. Carmen Green
00:07:01
There’s not really a benefit to having chronic pain. It steals. It’s a thief in the night. And it steals the lives and livelihoods and the quality of life for millions of people. If you have pain, we try and treat that pain and make people better to actually get them to the best health and well-being for them. And if you look at it from its impact on people, it actually is a real detriment. So if people say, well, gosh, they’re just making up, you should just suck it up, you should live with it. And it’s not that easy. We also know that the pain is also perceived in the brain. So it’s not all in your head. There are parts of the brain that actually light up when people have pain.
Dr. Sanjay Gupta
00:07:46
If I were to come see you and you’re trying to measure my pain.
Dr. Carmen Green
00:07:50
Yeah.
Dr. Sanjay Gupta
00:07:51
People are used to. If they’ve been in an emergency room, seeing the smiley face chart and saying, how would you, you know, sort of rate your your overall pain? How do you approach what seems to be a very subjective thing and try and make it objective?
Dr. Carmen Green
00:08:05
Yeah. So we don’t have a pain ometer. We don’t have something that says, boy, you definitely have pain. You don’t. It really does come to looking at the whole person. And so someone might come in to me and they say, you know, I’ve had pain for this many years. Hurts, my back hurts. And we start going through the history. What brought on the pain? What makes it better? What makes it worse?
Dr. Sanjay Gupta
00:08:29
Right.
Dr. Carmen Green
00:08:29
So there’s also that emotional component. So we always assess people from both a physical standpoint. You always do a good physical exam after you do the history. And then you also sort of look at what’s going on with them emotionally and socially. Most people are wanting someone to ask them about their pain. And so the number of times that I go into a patient’s room and they say, you know, Dr. Green, you’re the first person to ask me these questions. It’s astounding who is able to talk about their pain. How do we hear the pain complaints? So we got somebody handsome like yourself comes in with your, you know, your tie. We’re more likely to potentially hear your pain story. We call that physician variability in decision making. And also it’s also how the patient presents. Now, you add the whole race and ethnicity on that. And if you have a little bit of dirt underneath your nails, we may not be willing or able to hear that story as well.
Dr. Sanjay Gupta
00:09:36
That’s really powerful. I mean, you know, as you’re saying that I’m I’m imagining it and thinking, okay, am I susceptible to that myself? I got to tell you, this is a bit of a side note. My wife. I had a herniated disk. Now I’m a neurosurgeon. This is actually my area of expertize. And so she had pain. She was she’s a bit stoic about it and she’s telling me about it. But I’m not quite grasping for some time the degree of pain that she has. Long story short, is that she ends up getting an MRI and has a gigantic herniated disc, has to have it operated and does well after her operation. But I’m her husband. I’m a neurosurgeon. She had a problem that I trained to be able to recognize and take care of, and it kind of got by me a bit. If that can happen in my situation, I imagine as a pain doctor, it’s got to be really hard to again, be objective about something that is so subjective.
Dr. Carmen Green
00:10:43
Yeah, I think that you’re absolutely right, and I think every physician has had that type of experience, someone that they’ve loved, and they’re like, Really? What do you mean you’ve got a disc? And so when we can’t take care of the pain, so we can’t make the pain go away. How can we help people to live really whole and healthy lives? One of the things I’m I’m interested is the whole conversation about, you know, what happens to a person when they’ve not been believed for so long that they just sort of kind of suck it up. So, you know, pain is particularly difficult. And that’s reason why we need to have more pain medicine physicians and we need to, you know, before they train people. How to take care of pain in the in the primary care arena. And also, we need to educate patients on how to talk about pain with their doctor.
Dr. Sanjay Gupta
00:11:33
Can you predict somebody who’s going to be more vulnerable to pain versus someone else? Gender, age, life experience, anxiety scores.
Dr. Carmen Green
00:11:45
So we know that people who have more depression, have more anxiety, have worse pain, worse outcomes. So that’s reason why when we you come to a pain doctor like me, we always assess your sleep. We always assess your anxiety or depression. How do you deal with pain? Are you a person who tends to catastrophize? And if those are issues, then we try to address them early and reorient them in how to think about this pain. That this pain is not necessarily something that’s going to kill you, certainly interferes with your quality of life. We tend to get people involved with psychologists or social workers very early in a multidisciplinary pain center so that we can all sort of take our little piece. Pain is not a singular discipline. Right. So usually there’s a physical therapist involved. Usually there is a psychologist or a social worker involved. And we all are sort of involved in how do we get this patient to the best place for their for health and well-being.
Dr. Sanjay Gupta
00:12:44
Right. Do you think of pain as its own disease?
Dr. Carmen Green
00:12:48
Absolutely. So, you know, you have a patient with pain. The blood pressure can go up. You know, we see physical changes. It is a disease. And actually it is more prevalence in cardiovascular disease, diabetes combined. And the costs associated with pain, you know, the dollars, the medications is huge.
Dr. Sanjay Gupta
00:13:13
When we were covering the opioid epidemic, you know, it was one of these stories that I oftentimes felt was it was a tough story to tell, but it was a story that, you know, made sense. There was too many of these pills given out. It led to this problem of addiction. But oftentimes, many times, there was a side story which didn’t get told enough. And that is people who had legitimate pain, that were not abusers, who got caught in the crossfire of this entire opioid battle. They got demonized as people who, you know, were likely to become addicts. And at the same time, they didn’t get their pain addressed anymore. How big a problem is this, this whole opioid epidemic been on people who actually suffer from pain?
Dr. Carmen Green
00:14:01
It’s been tremendous and it’s been heartbreaking. The stories of people who’ve been on opioids for a long period of time, who lived high quality lives, were present for their kids, who never abused their medications, never lost a prescription, have been caught up into a system in which, all of a sudden, they may be viewed as drug addicts, particularly if you’re a person of color. So we have these stereotypes that are associated with who is going to abuse drugs. We have stigma associated with people who live with acute or chronic pain. We’ve criminalized opioids in black and brown people, and now we’ve normalized it in Caucasians. And so who do we think of as the addict? Right. So we know as relates to racial ethnic minorities, they have less access to health care regardless. They have less access to pain care. They receive less medication than Caucasians. We need to make certain that people who deserve care get high quality care and that can be done.
Dr. Sanjay Gupta
00:15:16
You’re a leading pain doctor in the country. Are you optimistic about the future of pain therapy? And you know just where we will be with pain five, ten years from now?
Dr. Carmen Green
00:15:26
I am. I’m hopeful that we will be able to embed some of these things into how we teach health care professionals, how to actively listen to people. There are many, many things that I have in my toolbox in order to take care of people with pain. Just the same way when you’re getting ready to work on somebody who has a brain cancer. Right. You have a multidisciplinary team that comes together, you know, to think about what is the best treatment for this particular person. What do we need to make certain that the patient has the best possible outcome? That’s what we need for pain.
Dr. Sanjay Gupta
00:16:04
You may have heard that term before. Interdisciplinary approach. It’s also called multimodal. Meaning the patient will receive several different types or modes of treatment for their pain. And this might actually hold the key to helping people with chronic pain. After the break, we’re going to hear from one patient who tried it out and got some pretty surprising results.
Dr. Sanjay Gupta
00:16:35
And now back to chasing life. You know, as a doctor myself, I can tell you that pain management is such an important part of the doctor patient relationship. How patients communicate their pain, how doctors respond to it and how we measure success are all very important parts of the equation. But things don’t always go according to plan. People can spend years searching for relief from their pain, and some even end up at specialized clinics.
Julianne Vasichek
00:17:06
Not paying was really affecting my life. I’d say it like an eight out of ten level. You know, it was very painful. It was causing me to lose sleep at night.
Dr. Sanjay Gupta
00:17:15
38 year old Julianne Vasichek has been suffering from chronic pain for over a decade. Growing up, she was an athlete, a former college hockey player, in fact. But around 2008, she developed a digestive disease that ended up leading to five abdominal operations, including a liver transplant. And she developed a pain that just wouldn’t go away. A few years ago, Julianne was referred to the Mayo Clinic’s Pain Rehabilitation Center, where she met Wesley Gilliam, the director of the program there.
Julianne, how have you been?
Julianne Vasichek
00:17:49
Better and better. I just told somebody the other day that I think I feel the best I’ve felt since I was about 21. So I found the fountain of youth.
Well, it’s pretty remarkable how far you’ve come, considering what you’ve been through.
Julianne Vasichek
00:18:05
Mm hmm. I think one of the biggest things about, like, havings pain is it makes you kind of pull back into yourself. It makes you disengage, it dissociates you from your social life and just your regular quality of life. So just changing that perspective makes such a difference. And you do more in the pain clinic in the first day than you’ve done, you know, frankly, in a long time. And you do it repeatedly and you’re just kind of amazed. Like once you make it through that first few days, you know what you’re doing.
Something we hear it all the time. The first day they say, How am I going to go from eight in the morning to four in the afternoon? And I’ve been spending, you know, a majority of my days in bed before I arrived here. I can’t possibly do that. And it’s quite something when people get through those first few days and you go, you remember a couple of days ago you said you didn’t think you’d be able to make it through a whole day. Congratulations. You just did three in a row.
Dr. Sanjay Gupta
00:18:57
Mayo’s pain rehab center offers a three week intensive program that gives patients new ways of thinking about their pain. They don’t promise that you’re going to leave pain free, but the program aims to restore function, that is, to teach patients how to return to the activities they used to do and improve their quality of life.
Any pain rehab model that you participate in, there’s a few of them around the country. There aren’t many. They’ll look subtly different. But the underlying fundamental principles of it are what we call functional restoration. So three primary modalities of any good pain rehab program are going to be physical therapy. All of our patients do an hour a day of PT, irrespective of how they feel, even when they’re not feeling particularly good and they’re hurting pretty badly, we still expect them to be working through physical therapy. To reinforce that movement is not something to avoid or to fear, even if you’re hurting.
Julianne Vasichek
00:19:50
Yeah, I would say it is. You know something that’s right in my line. I’ve worked as a strength and conditioning coach for a lot of my life and I’m now a hockey coach. But I realized, you know, with the abdominal pain, it was kind of giving me some hindrance towards, you know, really kind of, you know, pushing myself a little bit. So getting that regular stimulation and kind of making it fun too. And they brought in a hockey stick so I could do some stick handling there because I’m a hockey player. So kind of changing your perception that exercise doesn’t have to be this, you know, image that we see all the time in the world of people lifting big weights or running marathons. You know, it’s really just about getting some movement in.
Dr. Sanjay Gupta
00:20:29
In addition to physical therapy, patients at the pain rehab center also work with occupational therapists.
Occupational therapists are fabulous at finding alternative strategies for getting things done that can hopefully reduce pain for folks. But even if it generates a little bit of pain and gives them confidence, they can still do things. So we try to replicate real life as best we can. So our OTs will have groups on simple things like getting in and out of bed in ways that reduce the amount of strain that you might put on your low back for example, if you if you have back pain. How do we garden in a way that we want to getting down on the ground and or playing with your grandkids or your kids, just trying to approximate day to day movements that people, frankly, are avoiding because it’s become so associated with pain.
Julianne Vasichek
00:21:17
And I will just kind of jump in note like occupational therapy wise. You know, I wasn’t working at the time, I was on disability and so I wasn’t sure what it was going to be like to return to work. You know, what it was going to be like to work a full 8 hour day again. But they helped with recommending a standing desk so I could stand up and be a little more active and change my positioning. So I wasn’t kind of sitting in the same position all the time, and there was just a multitude of other little tips and tricks that I learned with occupational therapy to just adjust my life.
Dr. Sanjay Gupta
00:21:49
And then there’s the all important psychological component.
That’s kind of my role in the practice and psychology is about can we just start to look at What are you thinking about when you’re hurting? How can we help people manage their anxiety? Their mood states, which are big amplifiers of pain.
Julianne Vasichek
00:22:09
With the psychology piece. After a liver transplant, after you have all of your abdominal muscles cut. It’s hard to even just stand up straight. And so, you know, anybody who has surgery, you experience a difference in how your body operates and you might compensate by touching the area or even just thinking about the area. And so even me learning to not guard and have that reaction of pulling across my abdomen and more anymore, I think really changed my perception of the pain. And I think it was amazing for me to just realize that I was having these pain behaviors. And and maybe you can describe pain behaviors a little bit, Dr. Gilliam, and kind of how we reinforce those.
Sure. Yeah. Pain behaviors are always a tricky concept for folks because it’s it’s a bit in the abstract. Right. But basically, it’s these behavioral patterns that people fall into in response to their pain in an effort to make themselves more comfortable and to feel better. So these behaviors are very reinforcing because they, in a lot of cases, at least early on, serve a purpose of reducing pain, and they’re effective at doing that. So, for example, you might have somebody that just a pain behavior might just be simply, I’m going to avoid walking because when I walk, it hurts my back. So short term, that behavior is very effective because it alleviates discomfort in people. But long term, as you are restricting your movement and your activity, your body gets more deconditioned, you actually become less tolerant of pain or your pain threshold drops. So over time, things that didn’t hurt before and now they’re going to start to and I think that gets lost on a lot of people because we’re all kind of hardwired to want to avoid things that we don’t like. Pain being one of them. All of us are like that. And there is a real when you think about physical therapy for chronic pain, Julianne, I think you’ll probably agree with this. There is frankly a real psychology to that.
Julianne Vasichek
00:23:58
Yeah, we’re not going to be able to take pain away, you know, but it’s it’s getting you back to living a quality of life that that is functioning. And you’re not letting pain control your life, because that is certainly, I think, how it gets to be. You know, pain does make you very vulnerable. But I think if you’re willing to go into that vulnerability, you know, it’s possible to function well with pain and to have a good quality of life, even if your pain is just lessened. It’s possible, to still do the things that you think you can’t do.
Dr. Sanjay Gupta
00:24:30
It’s probably clear to you now from Julianne’s experiences that when it comes to tackling chronic pain, there is no one size fits all approach. That’s what I’m trying to convey to you here. Our understanding of this continues to evolve. Remember Steve, the guy who can’t feel pain? He and Julianne are in some ways like two sides of the same coin. And researchers believe his genetic condition could contain important clues about treating chronic pain like hers. Various pharmaceutical companies are now trying to create medications that can mute or switch off the pain signals in our bodies, essentially mimicking Steve’s condition. Now, there’s a lot baked into that, and it may be far off, but specialists like Dr. Carmen Green are hopeful about the future of pain medicine. I asked Dr. Green for advice for people struggling with chronic pain.
Dr. Carmen Green
00:25:22
Well, first of all, I would tell you, you don’t have to live with pain. There are many things that we can do to help people with pain. I think the other part is you need to advocate for yourself. And if you have difficulty advocating for yourself, then you need to bring an advocate with you. If you don’t like some of the responses and you need to go to another physician, another primary care provider who can help you and actually listen.
Dr. Sanjay Gupta
00:25:49
If nothing else, I hope today’s podcast has reminded people that if you have chronic pain, you should not give up hope. There’s a lot that’s being worked on now and a lot of promise that’s coming down the pike. But as a neurosurgeon myself, I’ve often taken care of patients who come in with extreme pain, and I’ve watched them transition from a life of despair, a life where they thought they had lost so many of the activities that they once were able to do, to a life where they feel much more optimistic, full of activity, full of energy, energy they thought was gone forever. It is possible and it is important not to give up hope.
Dr. Sanjay Gupta
00:26:31
We’ll be back Tuesday. Thanks for listening.
Dr. Sanjay Gupta
00:26:38
Chasing Life is a production of CNN audio. Megan Marcus is executive producer. Zoe Saunders is the senior producer. Our podcast is produced by Rachel Cohn, Jordan Gasspoore, Audrey Horwitz, Paige Sutherland and Grace Walker. Our production assistant is Allison Park. Our intern is Eduardo Ocampo. Our medical writer, Andrea Kane. Tommy Bazarian is our engineer and a special thanks to Ben Tinker and Amanda Sealey of CNN Health, as well as Ashley Lusk, Rafeena Ahmad, Courtney Coupe and Daniel Kantor from CNN Audio.
